COVID-19 1 year later: Pandemic ‘long haulers’ say surviving the virus is only half the battle
PHOENIX - We’re taking an in-depth look at Arizonans still dealing with the aftermath of the COVID-19 virus. They’ve recovered from the worst symptoms, yet they continue to suffer from potential long-term side effects several months later.
Meanwhile, doctors and researchers continue to study how the coronavirus is impacting the entire body.
Since the COVID-19 pandemic hit Arizona, more than 800,000 cases swept the state — stealth-like, sometimes swiftly, sometimes slowly, whether the numbers surged or steadily climbed.
A year later, we’re learning that surviving is only half the battle:
"My doctor, a few weeks ago, said now it’s time to start looking at this as more of a chronic issue."
Arizonans of all ages, with different backgrounds:
"I develop anxiety."
"I’m very active. I’m young."
Sharing the common denominator of beating COVID-19, yet still fighting the lingering effects of the virus that left their bodies.
"I just want to be medication free."
Haunted by symptoms they can’t shake.
"This is like nothing we’ve ever seen before."
They are the "long haulers" of the COVID-19 pandemic.
Adriana Soto
For 34-year-old Adriana Soto, she just wants the simplicities of her sense of taste and smell to return.
"OK, so this is cinnamon. And it doesn’t smell like what I remember it smelling like ... it has like, this spice like pepper kind of scent, like almost nothing."
Some things just don’t smell the same, even cleaning supplies.
"This doesn’t smell like a cleaner to me. This just smells like, I don’t know ... like if it was just liquid like water," said Soto.
And the morning fuel she’s been drinking for decades.
"I would make my morning coffee and I’d be like oh, OK, there’s a coffee coming ... and now it’s like it smells like dirt."
Coronavirus in Arizona: Latest case numbers
Despite getting COVID-19 last July and recovering, Soto says not only have her senses been impacted, she’s experiencing "brain fog" as working from home can be a mental challenge.
"I mean, I guess it has affected my performance. I mean, why even hide it, you know, on top of things and I’m asking for extensions on things, you know, that are coming due."
"Brain fog," or the difficulty concentrating is one of the long-term symptoms being reported, according to the Centers for Disease Control and Prevention. Fatigue, shortness of breath, body aches, heart palpitations, and even more serious issues affecting organ systems throughout the body. The complications can be cardiovascular, respiratory, and neurological.
"All these organs are still being affected and for a long period of time," said Dr. Heemesh Seth, a pulmonologist.
Affiliated with HonorHealth, Dr. Seth with the Arizona Pulmonary Specialists treats post-COVID patients. What he's studying starts in the lungs.
"Usually the virus will clear the body, but the inflammation stays, causes a lot of damage to the tissue and over time, it takes a lot longer for that inflammation to go away."
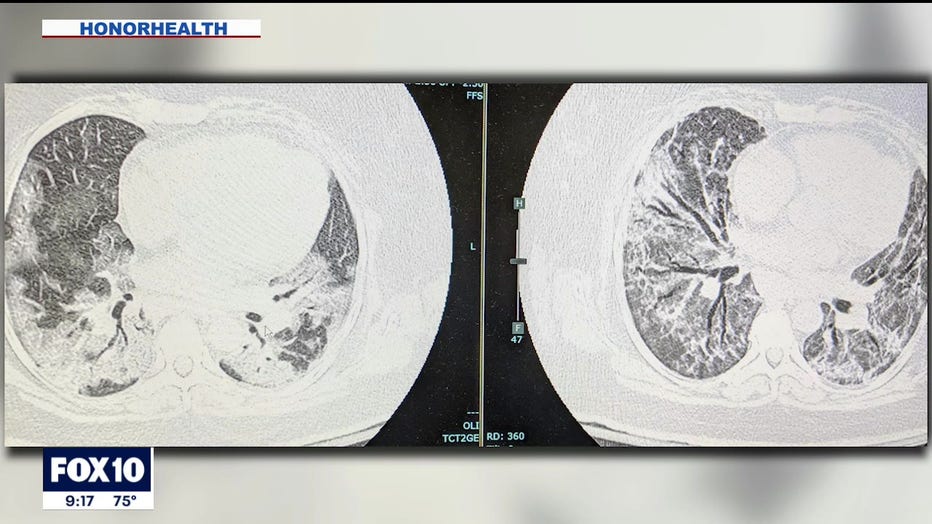
Dr. Seth looks at the haziness or patches in a CT scan, which shows one patient’s lungs. The image on the right was taken a month after the image on the left.
The images don’t look so different from each other — still showing inflammation and the development of scarring.
"Basically, the amount of lung that’s being damaged and that’s where patients need more and more oxygen."
MAP: Arizona Coronavirus cases by zip code
As for similarities between COVID lungs and smokers’ lungs, Seth says "what happens in smokers’ lungs is the damage happens over 30, 40, 50 years of smoking a pack a day or equivalent of that, but what we’re seeing in patients with COVID is they get very similar symptoms of severe shortness of breath, but within days to weeks."
Alyssa Lanoue
Recovery time can take several months. 41-year-old Alyssa Lanoue says she had COVID pneumonia back in December. She is now seeing a cardiologist.
"I could carry a load of laundry from my dryer to the couch to fold and my heart rate skyrockets into the 130s while on medication to regulate that."
Lanoue says she’s never been diagnosed with a heart condition before getting the coronavirus. Now it’s a daily grind to do chores.
"I’m still dealing with, like a lot of like, the fatigue and exhaustion and a lot of the brain fog," said 38-year-old Tiffany Jumper.
Jumper fought COVID-19 in an intensive care unit last summer. She was left with physical and mental side effects, experiencing post traumatic stress, even in her sleep, waking up from nightmares.
"Sometimes the dreams look like the families who were standing outside of the ICU and watching their loved ones in the windows or like when my family stood outside the windows of the ICU and I couldn’t touch them and I couldn’t feel them and I couldn’t be close to them and I was dying and I was suffocating and I wanted to say that I loved them and I couldn’t."

Tiffany Jumper
Jumper is hooked up to oxygen constantly, but now using four liters nightly instead of eight. As for her mind, train of thought can escape at any moment.
"I get really stuck now ... as a librarian and as a teacher ... I’m used to having the words, and I am used to having the vernacular."
Jumper can’t work in her current medical condition and her family’s support is vital.
Lanoue is on long-term disability after working in healthcare for more than 20 years. A sudden shift in lifestyle is difficult to grapple with.
"Just can’t turn that off. It’s been very hard for me and thank God my family, you know, listens to me cry about that, because I get very emotional when I talk about work."
Alexis Leal
For Alexis Leal, it took a decade to figure out why she was always fatigued and fainting.
"In sixth grade, I was 11 years old and one morning, I woke up and I fainted and that became my life."
The medical advice she usually received? Hydrate. By her early 20s, a doctor diagnosed her with Postural orthostatic tachycardia syndrome, known as POTS. The condition affects involuntary nervous system functions, such as heart rate and blood pressure.
"When I stand up, my blood flow goes all the way down to my legs and my legs swell, which causes me to lose oxygen in my head and that’s when I faint."
On top of POTS, Leal tested positive for COVID back in October. Several months later, both POTS symptoms and long-term COVID symptoms have compounded.
"On top of migraines and headaches, body aches — common symptom between the two, nausea, common symptom between the two, lightheadedness, dizziness, not able to answer questions right away," said Leal.
Doctors with Johns Hopkins medicine are researching similarities between those with POTS and long haulers: brain fog, increased heart rate, and severe chronic fatigue.
For now, it’s a marathon for health. Fighting to get back to their "normal," but also adapting to the aftermath of COVID-19.
"I think that really changes by the day to be honest. Recovery from COVID has been a lot of two steps forward, one step back," said Jumper.
The University of Arizona and Arizona State University are studying groups of people who have gone through COVID-19 and people who haven't. The goal is to see how long-term health is affected by the virus.
Online:
Dr. Heemesh Seth - https://azpulm.com/heemesh-seth-do.html
Arizona COVID-19 Long Haulers group
https://facebook.com/groups/arizonacovidlonghaulers
Continuing coverage of the COVID-19 pandemic:

Doctor offers advice for COVID-19 long haulers
There are some people who are still feeling the effects of COVID-19, months following their infection. FOX 10's Christina Carilla spoke with Dr. Peter Staats with the World Institute of Pain.
- Doctor: COVID-19 'long-haulers' not getting the attention they need
- COVID-19 long haulers share experiences of inhalers, hazy lung scans
- COVID-19 'long haulers' experience symptoms months after beating virus
In order to protect yourself from a possible infection, the CDC recommends:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
- Cover your mouth and nose with a cloth face cover when around others
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.
- Monitor your health daily


